Utilization Management Clinician LPN-2
Centene Corporation - Latham, NY
Utilization Management Clinician LPN-2

Oops! This job has expired, but don’t worry.
Explore other exciting job listings and take the next step in your career journey!
313
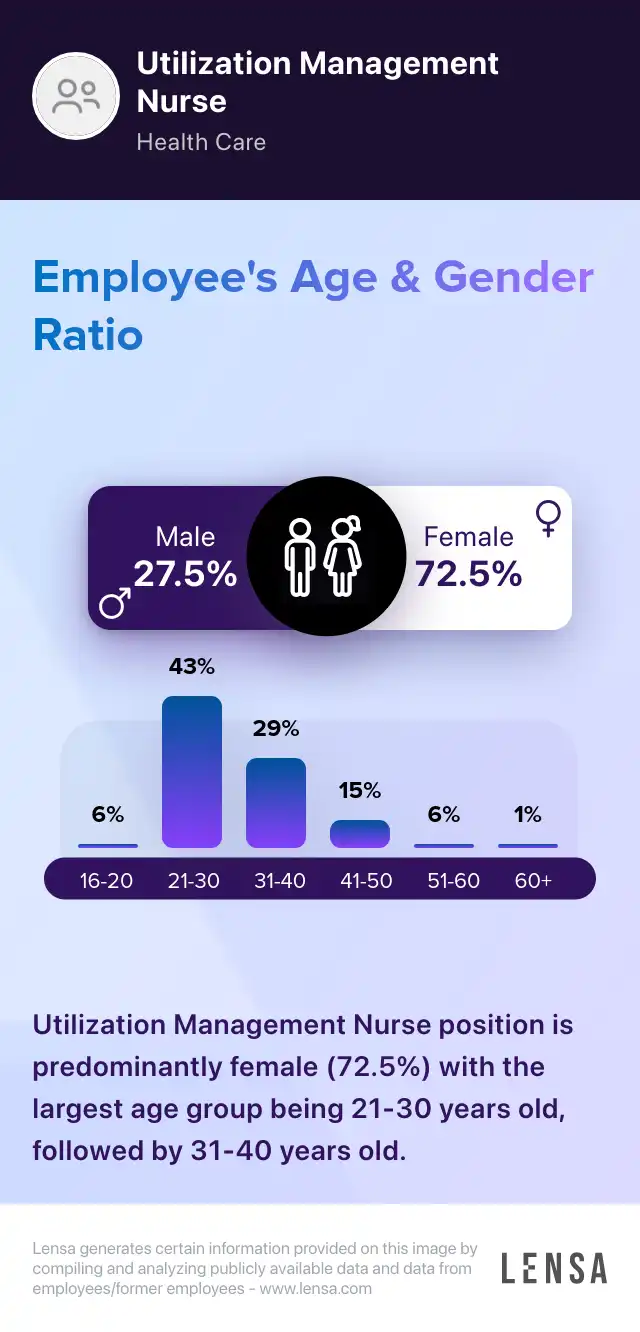
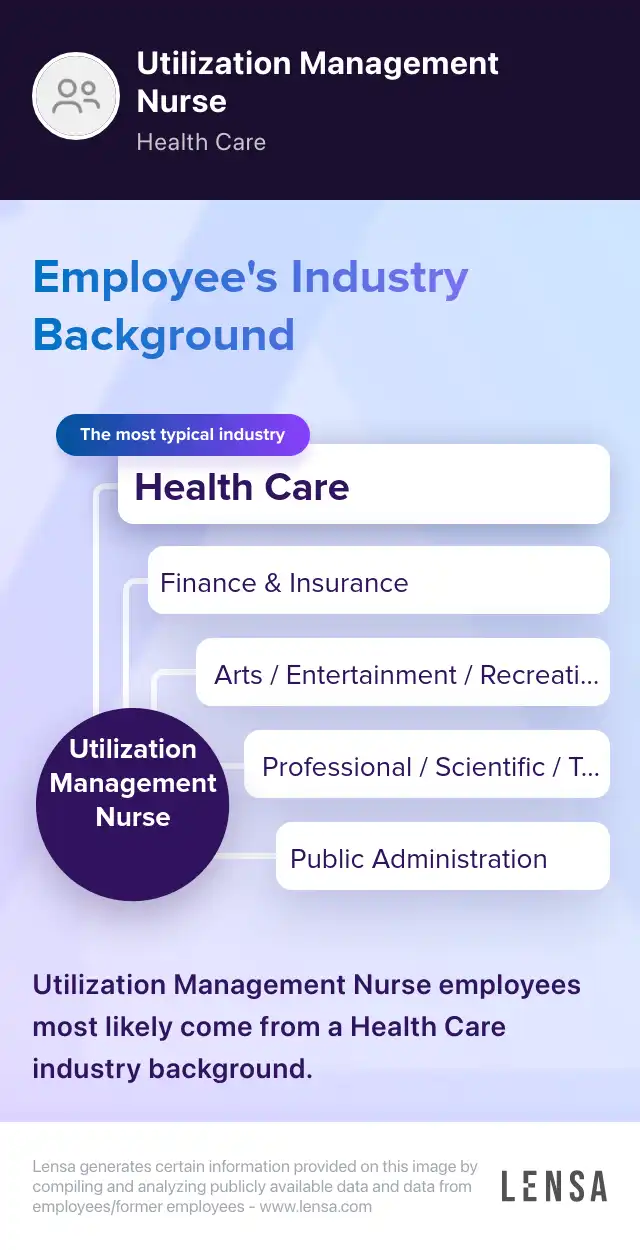
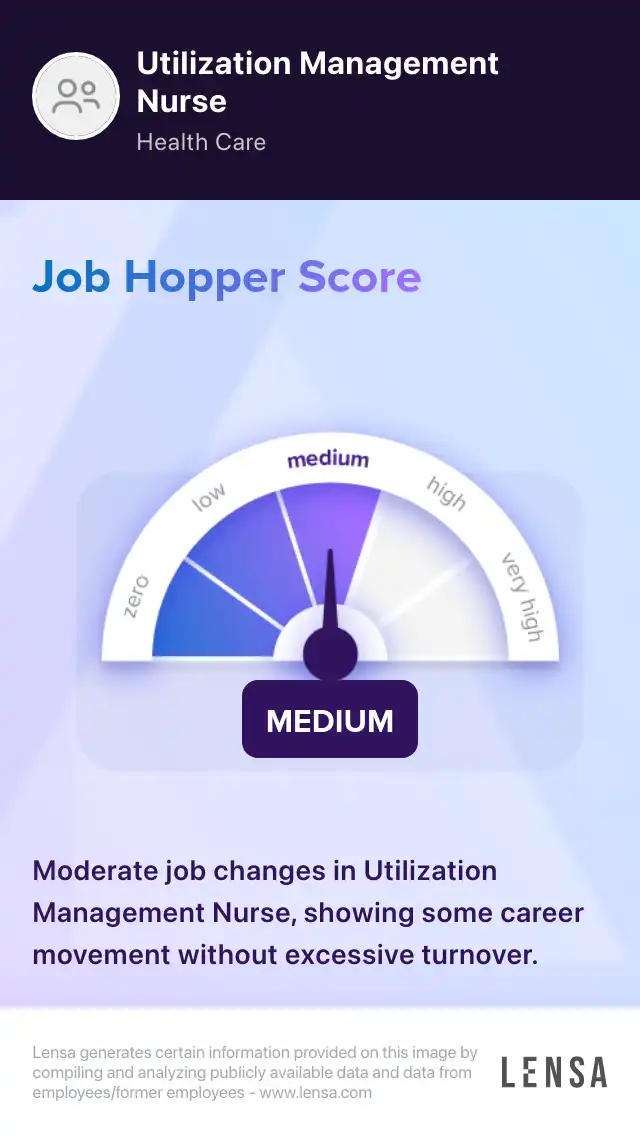
Utilization Management Nurse
jobs128
jobs in
Latham, NY
12
jobs at
Centene Corporation
Job
Company
Description
Salary
Skills
Benefits
Job Description
You could be the one who changes everything for our 26 million members as a clinical professional on our Medical Management/Health Services team. Centene is a diversified, national organization offering competitive benefits including a fresh perspective on workplace flexibility.
Position Purpose: The Utilization Review (UM) Clinician (LPN) performs clinical reviews to assess medical necessity of a broad range of outpatient and inpatient services, while maintaining compliance with all regulatory requirements.
Interfaces with medical directors, and both internal and external stakeholders, with regard to coverage for services, contract benefits and alternate resources available.
This position interfaces frequently with treating providers in the gathering of clinical information and may also provide education on the medical review process.
The Utilization Management clinician (LPN) makes coverage decisions based on specific criteria including Milliman.
Frequently collaborates with Fidelis medical directors in determining coverage of requested services.
Interacts with members to assist with accessing appropriate resources for requested services.
Education/Experience: Associate’s degree preferred; Bachelors Degree preferred. 1-3 years Utilization Review experience preferred. Managed care experience preferred
License/Certification: NYS LPN License Required
Our Comprehensive Benefits Package: Flexible work solutions including remote options, hybrid work schedules and dress flexibility, Competitive pay, Paid time off including holidays, Health insurance coverage for you and your dependents, 401(k) and stock purchase plans, Tuition reimbursement and best-in-class training and development.
Centene is an equal opportunity employer that is committed to diversity, and values the ways in which we are different. All qualified applicants will receive consideration for employment without regard to race, color, religion, sex, sexual orientation, gender identity, national origin, disability, veteran status, or other characteristic protected by applicable law.
TITLE: Utilization Management Clinician LPN-2
LOCATION: Latham, New York
REQNUMBER: 1365196
This job was posted on Sun Oct 16 2022 and expired on Tue Nov 08 2022.
Find out how you match this company


Centene Corporation
Finance & Insurance Companies & Insurance Agency & Brokerage Firms
Reviews
Summary
Centene Corporation is a Fortune 500 enterprise serving as an intermediary for both government-sponsored and privately insured health care programs. The main lines of Centene include Medicaid, where it is the largest provider in the country; ACA health insurance marketplace plans (under the Ambetter brand); Medicare; Tricare and traditional commercial insurance. The corporation's foundational belief is that everyone deserves access to high-quality, affordable healthcare with dignity. Working for Centene, you are offered a competitive benefits package, continuous development plans and opportunities (through Centene University) as well as retirement plans. The company puts an emphasis on sustainability from energy-efficient buildings to enterprise-wide recycling efforts as well as meals based on locally sourced ingredients for employees. Through the Centene Charitable Foundation, the company invests in organizations and institutions that improve the lives of local communities, with a focus on holistic wellness.
How do you prioritize your workload as a Utilization Management Nurse?
Answer
I prioritize my workload by assessing the urgency of each case and considering the potential impact on patient care.
How do you handle difficult conversations with patients or healthcare providers?
How do you ensure compliance with healthcare regulations and policies?

About the Utilization Management Nurse role
Registered Nurses Utilization Management Nurse
As Utilization Management Nurses, we coordinate the medical services provided by the facility. We make concise documentation of benefit management programs. We review the clinical information of patients. Monitoring the staff members of the facility is a duty of ours. We identify ways to prevent complications. We maintain clear, updated records of patient interactions. Utilization Management Nurses ensure that health care services are implemented effectively. We constantly review the treatment files of patients. We ensure that only the necessary procedures are administered. Determining the right amount of hospital stays is part of our duties.
Core tasks:
- coordinating the discharge process of patients
- preparing regular reports on patient management
- providing updates to the manager in charge of utilization management daily
- advocating the administration of quality care
313 Utilization Management Nurse jobs in Latham, NY

Similar jobs in the area