Please wait.

Utilization Management Rep I
Aerotek - Latham, NY
Utilization Management Rep I

Oops! This job has expired, but don’t worry.
Explore other exciting job listings and take the next step in your career journey!
313
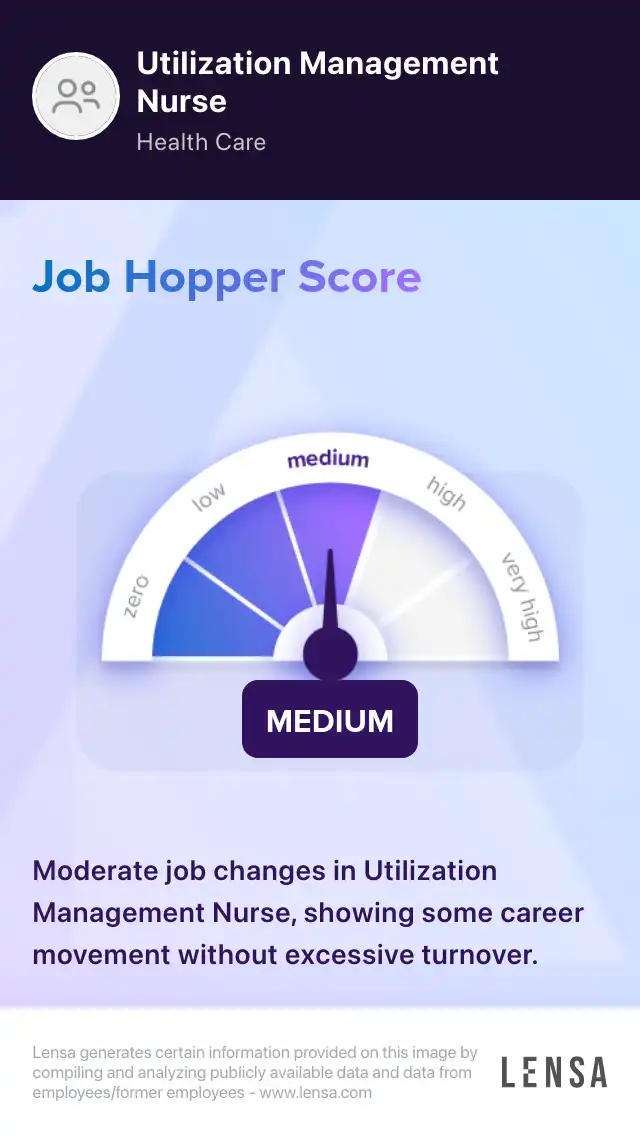
Utilization Management Nurse
jobs128
jobs in
Latham, NY
22
jobs at
Aerotek
Job
Company
Description
Salary
Skills
Job Description
Aerotek is hiring Medical Customer Service Representatives to assist a healthcare client in the Albany area. Representatives are responsible for coordinating cases for precertification and prior authorization review. Representatives take calls from providers and customers and verify that the patients are authorized for certain procedures.
Job Duties:
-
Filing and faxing of authorization entries.
-
Sorting faxes along with processing pre-authorization notifications.
-
Managing incoming calls or incoming post services claims work.
-
Determine contract and benefit eligibility and provide authorization for inpatient admission.
-
Responsible for the identification and data entry of referral requests into the UM system.
-
Check benefits for facility based treatment.
Additional Skills & Qualifications:
-
High speed internet with ethernet hookup.
-
Must have a private area to work in.
-
High School Diploma/GED.
-
Open to working on Weekends if needed.
About Aerotek:
We know that a company's success starts with its employees. We also know that an individual's success starts with the right career opportunity. As a Best of Staffing® Client and Talent leader, Aerotek's people-focused approach yields competitive advantage for our clients and rewarding careers for our contract employees. Since 1983, Aerotek has grown to become a leader in recruiting and staffing services. With more than 250 non-franchised offices, Aerotek's 8,000 internal employees serve more than 300,000 contract employees and 18,000 clients every year. Aerotek is an Allegis Group company, the global leader in talent solutions. Learn more at Aerotek.com.
The company is an equal opportunity employer and will consider all applications without regards to race, sex, age, color, religion, national origin, veteran status, disability, sexual orientation, gender identity, genetic information or any characteristic protected by law.
This job was posted on Thu May 06 2021 and expired on Mon May 24 2021.
Find out how you match this company


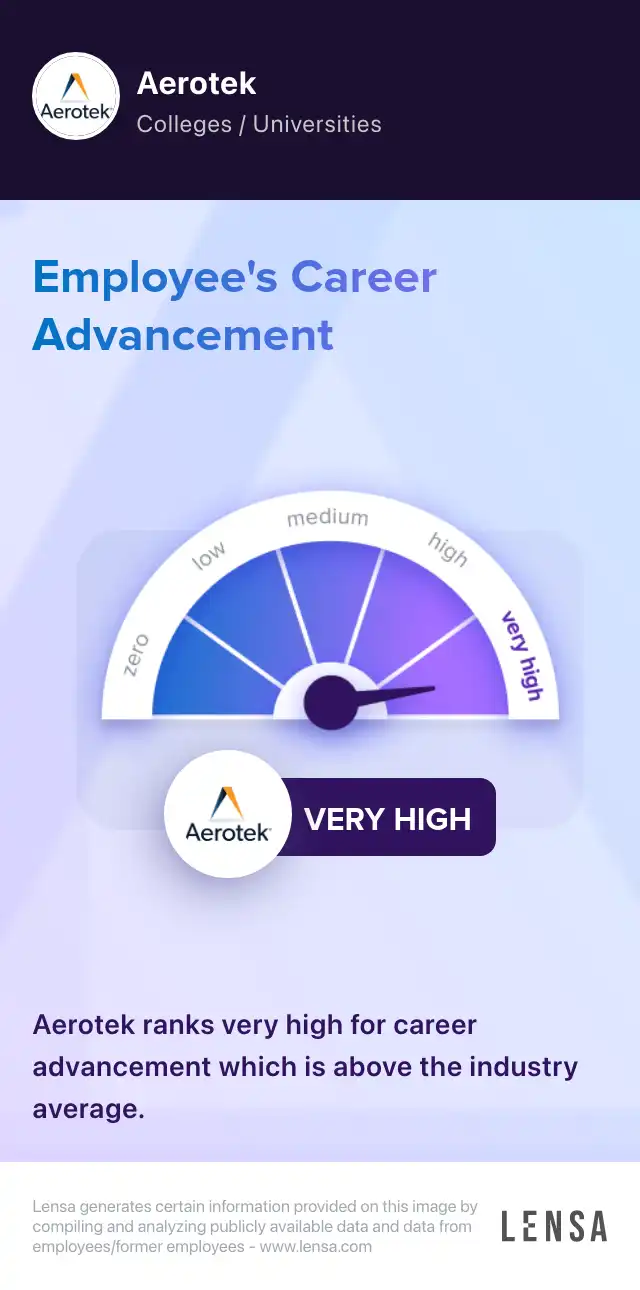
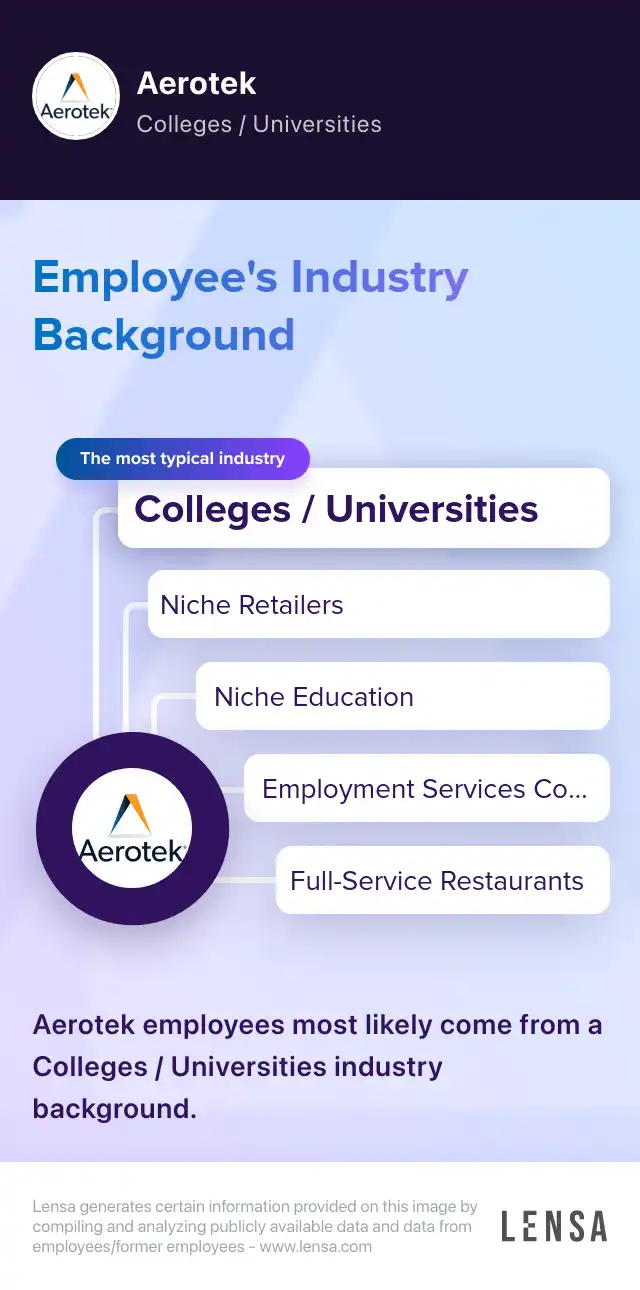
Aerotek
Employment Services Companies & Consulting Companies
Reviews
Summary
Aerotek, the Hanover, Maryland-based recruiting and staffing agency, offers workforce management services as well as short-term, seasonal staffing solutions within a wide range of industries including accounting, administrative & support services, environmental, and financial services. Diversity and inclusion is at the forefront of the Aerotek core values. Its corporate culture is rooted in guiding principles to build and nurture quality relationships that allows Aerotek to connect people with jobs. As ab Aerotek employee, the company will offer you benefits including national PPO with dental and vision, life insurance, accidental death & dismemberment and disability, a 401(k) plan, and paid time off. Via the Employee Discount Program, you might have access to discounts on car rentals, electronics, entertainment, fashion, travel and several other services.
How do you prioritize your workload as a Utilization Management Nurse?
Answer
I prioritize my workload by assessing the urgency of each case and considering the potential impact on patient care.
How do you handle difficult conversations with patients or healthcare providers?
How do you ensure compliance with healthcare regulations and policies?

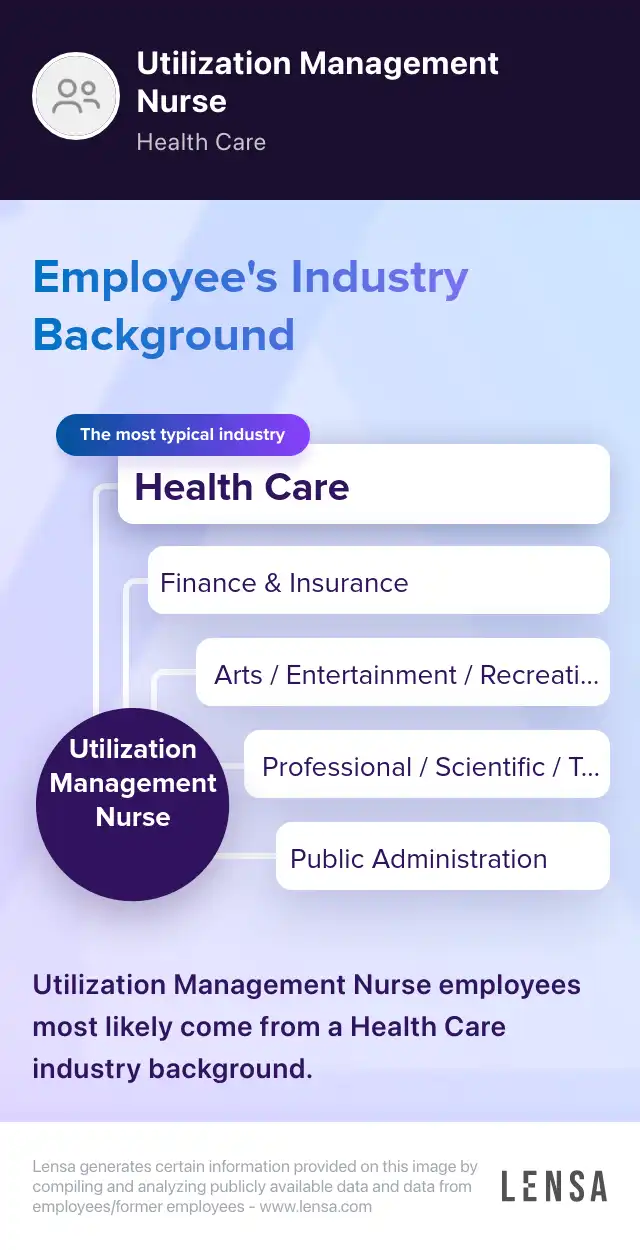
About the Utilization Management Nurse role
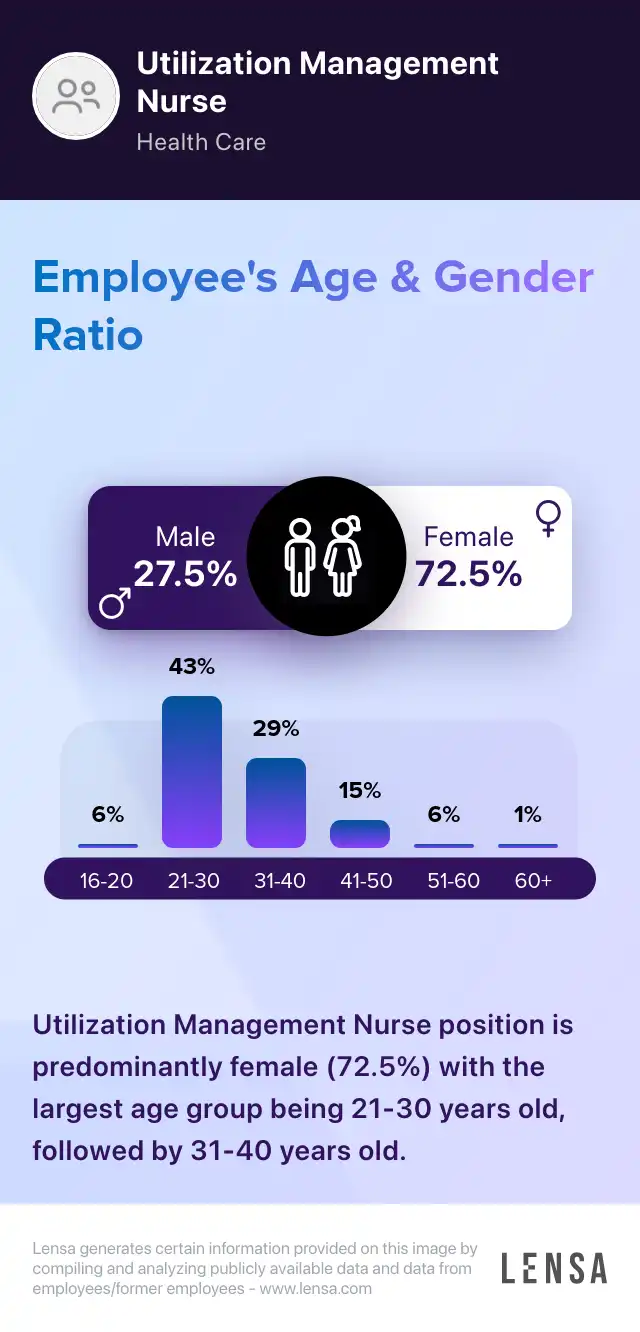
Registered Nurses Utilization Management Nurse
As Utilization Management Nurses, we coordinate the medical services provided by the facility. We make concise documentation of benefit management programs. We review the clinical information of patients. Monitoring the staff members of the facility is a duty of ours. We identify ways to prevent complications. We maintain clear, updated records of patient interactions. Utilization Management Nurses ensure that health care services are implemented effectively. We constantly review the treatment files of patients. We ensure that only the necessary procedures are administered. Determining the right amount of hospital stays is part of our duties.
Core tasks:
- coordinating the discharge process of patients
- preparing regular reports on patient management
- providing updates to the manager in charge of utilization management daily
- advocating the administration of quality care
313 Utilization Management Nurse jobs in Latham, NY

Similar jobs in the area