Please wait.

UM Clinician - BH
Aetna - Albuquerque, NM
UM Clinician - BH

Oops! This job has expired, but don’t worry.
Explore other exciting job listings and take the next step in your career journey!
313
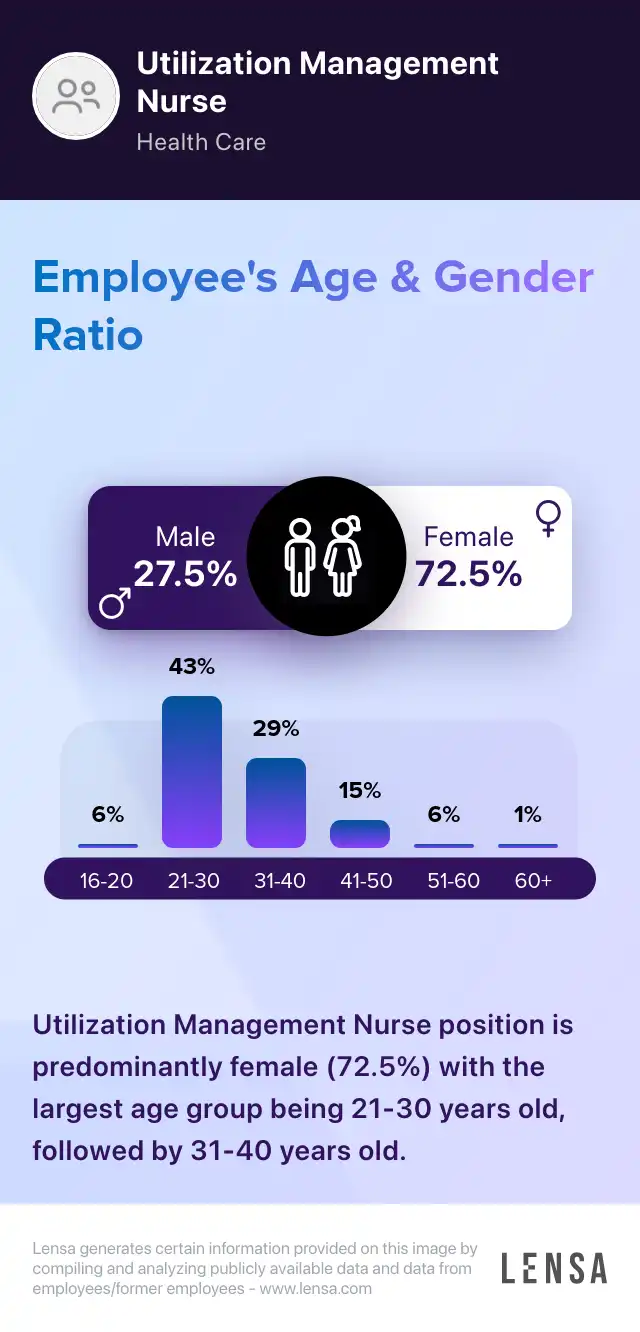
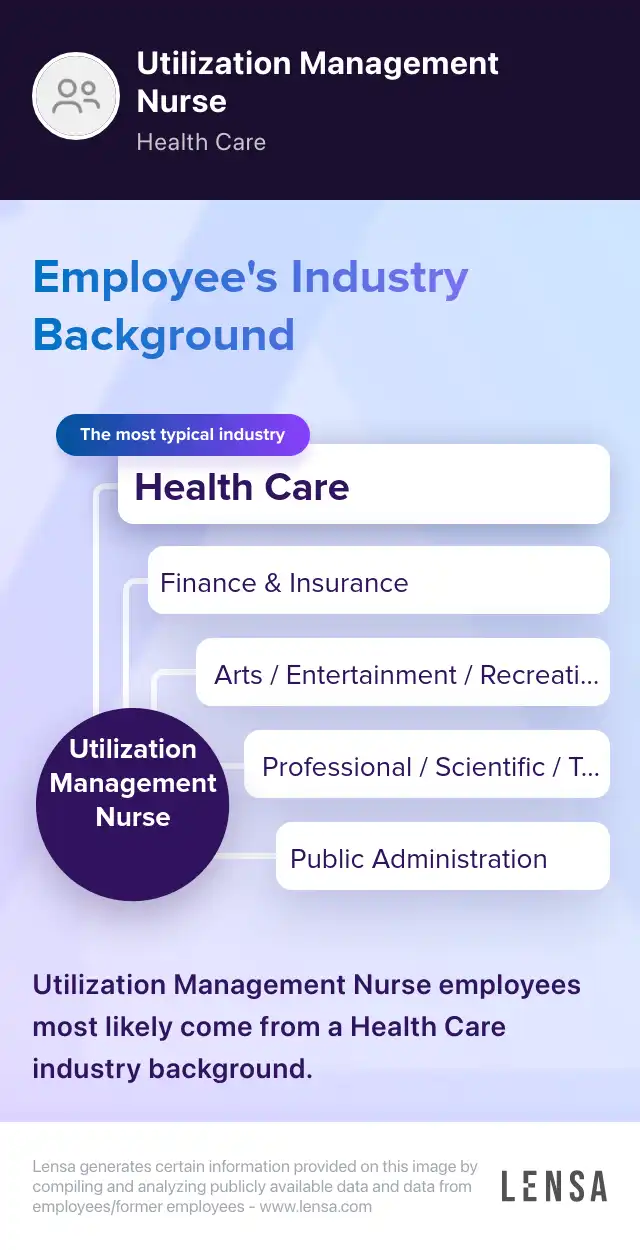
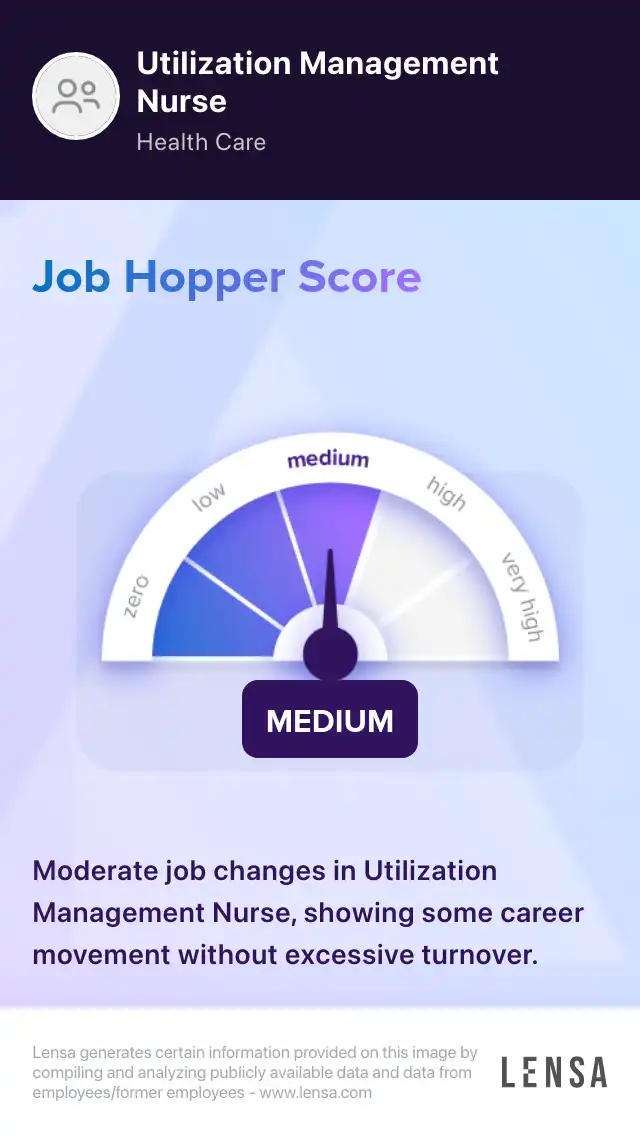
Utilization Management Nurse
jobs107
jobs in
Albuquerque, NM
17
jobs at
Aetna
Job
Company
Description
Salary
Skills
Benefits
Job Description
Req ID: 60102BR
Job Description
Full time work from home. Preference to those in Mountain or Pacific standard time.
POSITION SUMMARY
The Aetna Autism Care Team works within an integrated team to perform utilization review, as well as proactive discharge planning. This includes working in close collaboration with our business partners, as well as the enterprise to promote overall wellness for our members. A license to practice in the state in which you live is required.
Fundamental Components included but are not limited to:
Applies critical thinking and is knowledgeable of evidence-based treatment and clinical practice guidelines for Behavioral Health. The majority of time is spent at a desk and on telephonic or records review of precertification/concurrent/retrospective cases with the treating provider/records using specific criteria and making decisions to authorize services for our members OR refer to a physician for a determination. These clinicians also collaborate with providers/facilities to ensure appropriate planning to meet member needs.
Qualifications Requirements and Preferences:
Behavioral Health licensure required
3+ years clinical experience post-Master's degree required
Experience with children is a requirement
Autism experience is highly preferred
Utilization review experience preferred
Managed care experience preferred
Crisis intervention skills preferred
Position requires proficiency with computer skills which includes navigating multiple systems and keyboarding
Sedentary work involving periods of sitting, talking, listening. Work requires sitting for extended periods, talking on the telephone and typing into the computer
EDUCATION
The minimum level of education desired for candidates in this position is a Bachelor's degree or equivalent experience.
LICENSES AND CERTIFICATIONS
Mental Health/Licensed Clinical Social Worker
Mental Health/Licensed Professional Counselor
Nursing/Registered Nurse
Mental Health/Licensed Psychologist
Additional Job Information:
This is an opportunity to be part of a high performing dynamic team while enjoying the flexibility of working from home.
Benefit Eligibility
Benefit eligibility may vary by position. Click here to review the benefits associated with this position.
Job Function: Health Care
Aetna is an Equal Opportunity/Affirmative Action employer. All qualified applicants will receive consideration for employment without regard to race, color, religion, sex, sexual orientation, gender identity, national origin, disability, or protected Veterans status.
This job was posted on Fri Sep 13 2019 and expired on Wed Sep 18 2019.
Find out how you match this company


Aetna
Direct Insurance Companies
Reviews
Summary
Aetna is a managed healthcare firm offering traditional and consumer directed healthcare insurance and related services, with its headquarters in Hartford, CT. The company is committed to providing individuals, employers, healthcare professionals, and others with innovative benefits, products and solutions. Aetna is driven by the core values of integrity, excellence, caring, and inspiration. Through continual innovation, openness, and collaboration, Aetna connects people with new health and well-being approaches. If you would like to be part of a dynamic workforce and join a team where everyone works together to create a healthier world, Aetna will provide the benefits you need to keep thriving and advancing in your life and career. Working for Aetna will get you access to a broad range of perks from free yoga classes and a Healthy Lifestyle program to 401(k) and tuition and student loan reimbursement programs.
How do you prioritize your workload as a Utilization Management Nurse?
Answer
I prioritize my workload by assessing the urgency of each case and considering the potential impact on patient care.
How do you handle difficult conversations with patients or healthcare providers?
How do you ensure compliance with healthcare regulations and policies?

About the Utilization Management Nurse role
Registered Nurses Utilization Management Nurse
As Utilization Management Nurses, we coordinate the medical services provided by the facility. We make concise documentation of benefit management programs. We review the clinical information of patients. Monitoring the staff members of the facility is a duty of ours. We identify ways to prevent complications. We maintain clear, updated records of patient interactions. Utilization Management Nurses ensure that health care services are implemented effectively. We constantly review the treatment files of patients. We ensure that only the necessary procedures are administered. Determining the right amount of hospital stays is part of our duties.
Core tasks:
- coordinating the discharge process of patients
- preparing regular reports on patient management
- providing updates to the manager in charge of utilization management daily
- advocating the administration of quality care
313 Utilization Management Nurse jobs in Albuquerque, NM

Similar jobs in the area