Please wait.

Manager Contract Negotiation
CVS Health - Abbottstown, PA

Oops! This job has expired, but don’t worry.
Explore other exciting job listings and take the next step in your career journey!
485
Manager
jobs104
jobs in
Abbottstown, PA
36
jobs at
CVS Health
Job
Company
Description
Salary
Skills
Benefits
Job Description
Bring your heart to CVS Health Every one of us at CVS Health shares a single, clear purpose: Bringing our heart to every moment of your health. This purpose guides our commitment to deliver enhanced human-centric health care for a rapidly changing world. Anchored in our brand — with heart at its center — our purpose sends a personal message that how we deliver our services is just as important as what we deliver. Our Heart At Work Behaviors™ support this purpose. We want everyone who works at CVS Health to feel empowered by the role they play in transforming our culture and accelerating our ability to innovate and deliver solutions to make health care more personal, convenient and affordable.
Position Summary
∙ Negotiates, executes, conducts high level review and analysis of dispute resolution and/or settlement negotiations of contracts with larger and more complex, market/regional/national based group/system providers including but not limited to large PCP groups, pediatricians, advanced specialist groups, hospital based providers, ancillary providers, ambulatory surgical centers, behavioral health providers, etc. in accordance with company standards in order to maintain and enhance provider networks while meeting and exceeding accessibility, quality and financial goals and cost initiatives.∙ Recruit providers as needed to ensure attainment of network expansion goals, achieve regulatory and/or internal adequacy targets.∙ Support health plan with expansion initiatives or other contracting activities as needed.∙ Initiates, coordinates and own the contracting activities to fulfillment including receipt and processing of contracts and documentation and pre- and post-signature review of contracts and language modification according to Aetna’s established policies.∙ Responsible for auditing, building, and loading contracts, agreements, amendments and/or fee schedules in contract management systems per Aetna’s established policies. .∙ Conducts research, analysis and/or audits to identify issues and propose solutions to protect data, contract integrity and performance.∙ Manages contract performance and supports the development and implementation of value-based contract relationships in support of business strategies.∙ Collaborates cross-functionally to manage provider compensation and pricing development activities, submission of contractual information, and the review and analysis of reports as part of negotiation and reimbursement modeling activities.∙ Provides Subject Matter Expert support for questions related to recruitment initiatives, contracting, provider issues/resolutions, related systems and information contained.∙ Provide guidance and share expertise to others on the team.∙ Understanding of Value Based contracting and negotiations∙ Manage high level projects and recruitment initiatives with interdepartmental resources and/or cross functional stakeholders.∙ May participates in JOC meetings.∙ Supports or assists with operational activities that may include, but are not limited to, database management and contract coordination.∙ Organizing and transforming information into comprehensible structures.∙ Using data to predict trends in the customer base and the consumer population as a whole∙ Performing statistical analysis of data.∙ Using tools and techniques to visualize data in easy-to-understand formats, such as diagrams and graphs.∙ Preparing reports and presenting these to leadership.∙ Engage with providers and quickly move the providers though contracting processes in order to ensure meeting network adequacy requirements.
Required Qualifications ∙ 5-10 years of network contracting/management experience.∙ Ability to travel as needed (up to 25% travel).∙ 5 years of proven knowledge of standard provider contracts, terms and language desired.∙ 5 years of solid negotiating and decision-making skills while executing national, regional, or market level strategies.∙ In-depth knowledge of the managed care industry and practices, as well as a strong understanding of Aetna competitor strategies, practices, and financial/contracting arrangements.∙ Demonstrated high proficiency with personal computer, mouse, keyboard and all MS Office suite applications (e.g., Outlook, Word, Excel, etc.). Preferred Qualifications ∙ Knowledge of Medicaid programs and related subject matter preferred.∙ Solid decision-making skills while executing national, regional, and market level strategies.∙ Ability to forge long-lasting relationship.∙ Possess critical thinking, problem resolution and interpersonal skills.∙ Ability to forge long-lasting relationship.∙ Must possess critical thinking, problem resolution and interpersonal skills.∙ Ability to identify and capitalize on opportunities to support program delivery.∙ Communication Skills - Strong communication skills (written, verbal and presentation).∙ Ability to forge long-lasting relationships with providers.∙ Highly organized and self-driven. Education .Bachelor's degree desired or equivalent work experience
Pay Range
The typical pay range for this role is:
$54,300.00 - $136,500.00
This pay range represents the base hourly rate or base annual full-time salary for all positions in the job grade within which this position falls. The actual base salary offer will depend on a variety of factors including experience, education, geography and other relevant factors. This position is eligible for a CVS Health bonus, commission or short-term incentive program in addition to the base pay range listed above. In addition to your compensation, enjoy the rewards of an organization that puts our heart into caring for our colleagues and our communities. The Company offers a full range of medical, dental, and vision benefits. Eligible employees may enroll in the Company’s 401(k) retirement savings plan, and an Employee Stock Purchase Plan is also available for eligible employees. The Company provides a fully-paid term life insurance plan to eligible employees, and short-term and long term disability benefits. CVS Health also offers numerous well-being programs, education assistance, free development courses, a CVS store discount, and discount programs with participating partners. As for time off, Company employees enjoy Paid Time Off (“PTO”) or vacation pay, as well as paid holidays throughout the calendar year. Number of paid holidays, sick time and other time off are provided consistent with relevant state law and Company policies. For more detailed information on available benefits, please visit jobs.CVSHealth.com/benefits
CVS Health requires certain colleagues to be fully vaccinated against COVID-19 (including any booster shots if required), where allowable under the law, unless they are approved for a reasonable accommodation based on disability, medical condition, religious belief, or other legally recognized reasons that prevents them from being vaccinated.
You are required to have received at least one COVID-19 shot prior to your first day of employment and to provide proof of your vaccination status or apply for a reasonable accommodation within the first 10 days of your employment. Please note that in some states and roles, you may be required to provide proof of full vaccination or an approved reasonable accommodation before you can begin to actively work.
CVS Health is committed to recruiting, hiring, developing, advancing, and retaining individuals with disabilities. As such, we strive to provide equal access to the benefits and privileges of employment, including the provision of a reasonable accommodation to perform essential job functions. CVS Health colleagues can initiate a request for a reasonable accommodation, including a qualified interpreter, written information in other formats, translation or other services through myHR (1-888-694-7287, or through myLeave at myHR). If you have a speech or hearing disability, please call 7-1-1 to utilize Telecommunications Relay Services (TRS). We will make every effort to respond to your request within 48 business hours and do everything we can to work towards a solution.
This job was posted on Mon Oct 16 2023 and expired on Sat Oct 21 2023.
Find out how you match this company


CVS Health
General Hospitals & Outpatient Care Centers
Reviews
Summary
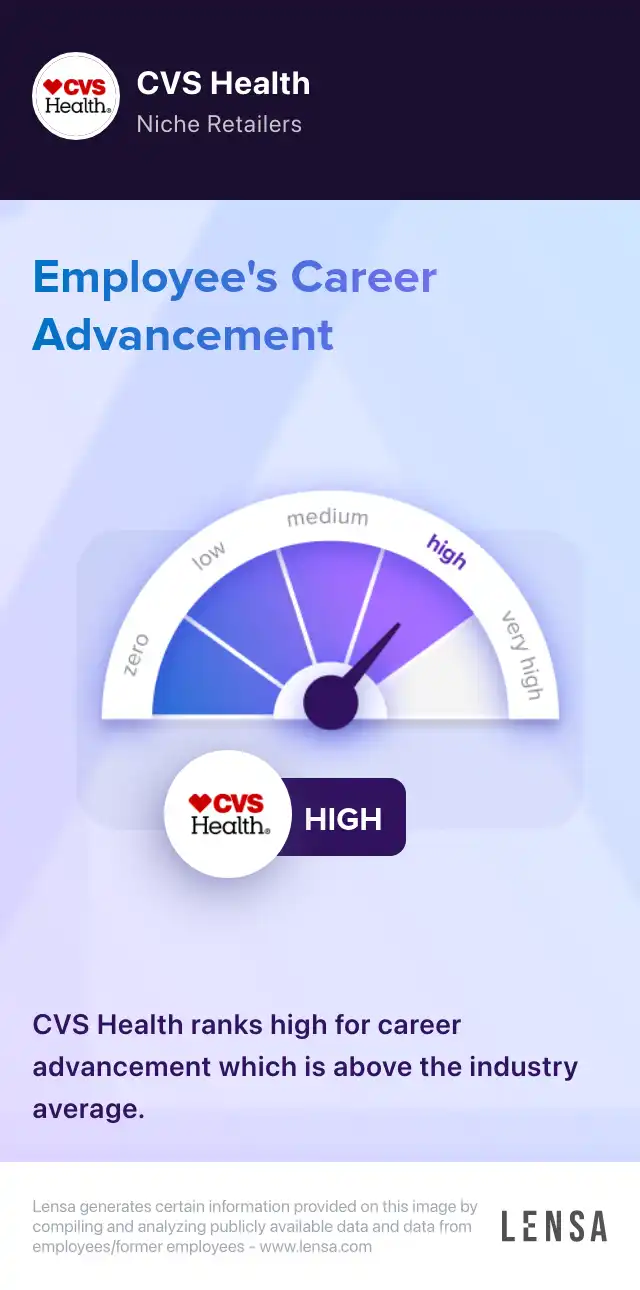
CVS Health, the Woonsocket, Rhode Island-based healthcare company, offers clinical, retail pharmacy, specialty pharmacy, pharmacy benefit management, and prescription mail order services in the US, the District of Columbia, and Puerto Rico. CVS’ mission is to provide people assistance on their path to better health, making quality care more affordable, accessible, simple and seamless.The company seeks to attract individuals whose beliefs and behaviors are in alignment with CVS core values of collaboration, innovation, caring, integrity and accountability. The multi-award winning company (e.g. Military Friendly Employer, America’s Top Corporation for Women Business Enterprises) provides opportunities to a diverse work experience that empowers the team for career success. CVS offers a benefits package to its employees, including medical, prescription, dental and vision coverage, a company contribution to a health savings account (HSA), employee stock purchase plan, adoption benefits, life, accident and disability insurance, paid time off, tuition reimbursement, and colleague discount.
How do you handle conflicts within your team?
Answer
I believe in open communication and addressing conflicts directly. I encourage team members to express their concerns and work towards finding a resolution together.
How do you prioritize tasks and manage your time effectively?
How do you motivate and inspire your team?

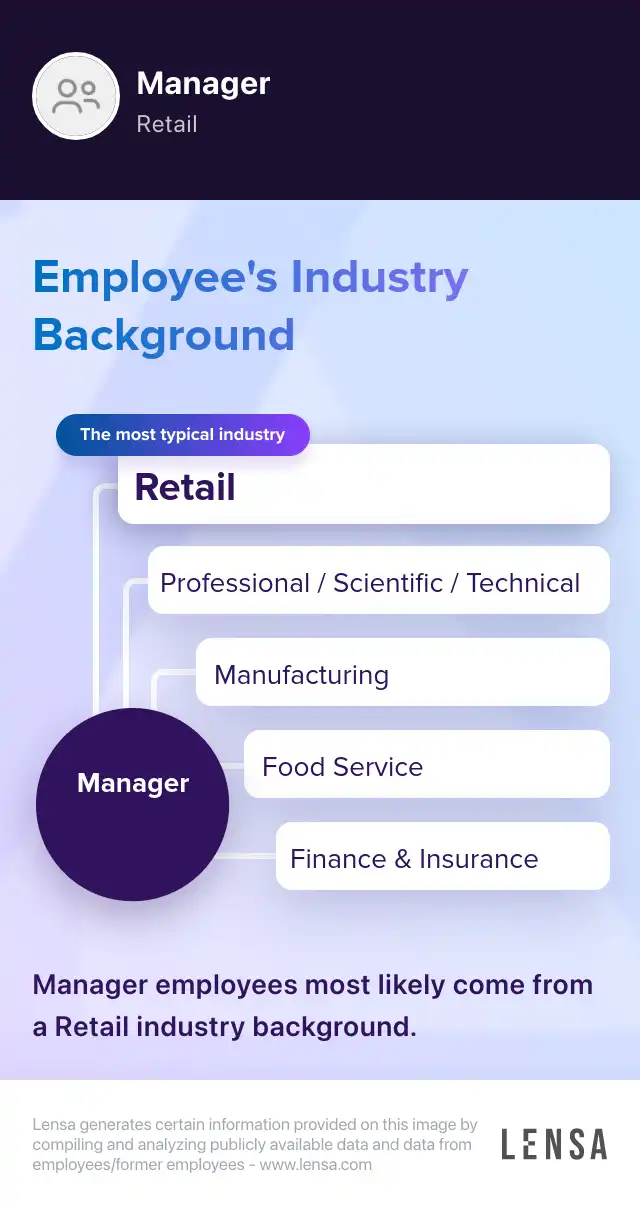
About the Manager role
General and Operations Managers Manager
As Managers, we are charged with overseeing a team or a department. We ensure staffing, adherence to quality and service standards, revenue increase, and market share. Our key accountability is to accomplish business goals. Our role covers a broad spectrum of responsibilities, but we generally hire and train employees, monitor problems, develop and implement business strategies.
Core tasks:
- supervise operations
- hire and train employees
- resolve conflicts and complaints
- achieve business objectives
- ensure adherence to company policies and procedures
485 Manager jobs in Abbottstown, PA

Similar jobs in the area